Understanding The Planned Abdominal Surgery Reasons
Planned abdominal surgery is a significant medical procedure that requires careful consideration and planning. Various factors may lead to the decision to undergo such surgery, and understanding these reasons is crucial for anyone facing this life-changing event. From chronic conditions to acute emergencies, the necessity for abdominal surgery can stem from a variety of medical issues that affect the digestive organs, reproductive system, and other vital structures within the abdomen. Patients often find themselves navigating a complex journey filled with questions about their health, the surgical procedure, and the expected outcomes. Whether it is due to a diagnosis of cancer, the presence of gallstones, or the need for a hernia repair, recognizing the underlying reasons for planned abdominal surgery can empower patients to make informed decisions in coordination with their healthcare providers.
In addition to the physical implications of undergoing surgery, there are emotional and psychological factors at play. The prospect of surgery can provoke anxiety, fear, and uncertainty. Therefore, having a clear understanding of the planned abdominal surgery reasons can help alleviate some of these concerns. By exploring the motivations behind the need for surgery, patients can better prepare themselves mentally and emotionally, leading to a more positive surgical experience and recovery process.
This article aims to delve into the various planned abdominal surgery reasons, providing insights into the common conditions and scenarios that lead to surgical intervention. By addressing frequently asked questions and outlining the processes involved, we hope to equip readers with the knowledge they need to navigate their own or their loved one's surgical journey with confidence.
What are the Common Reasons for Planned Abdominal Surgery?
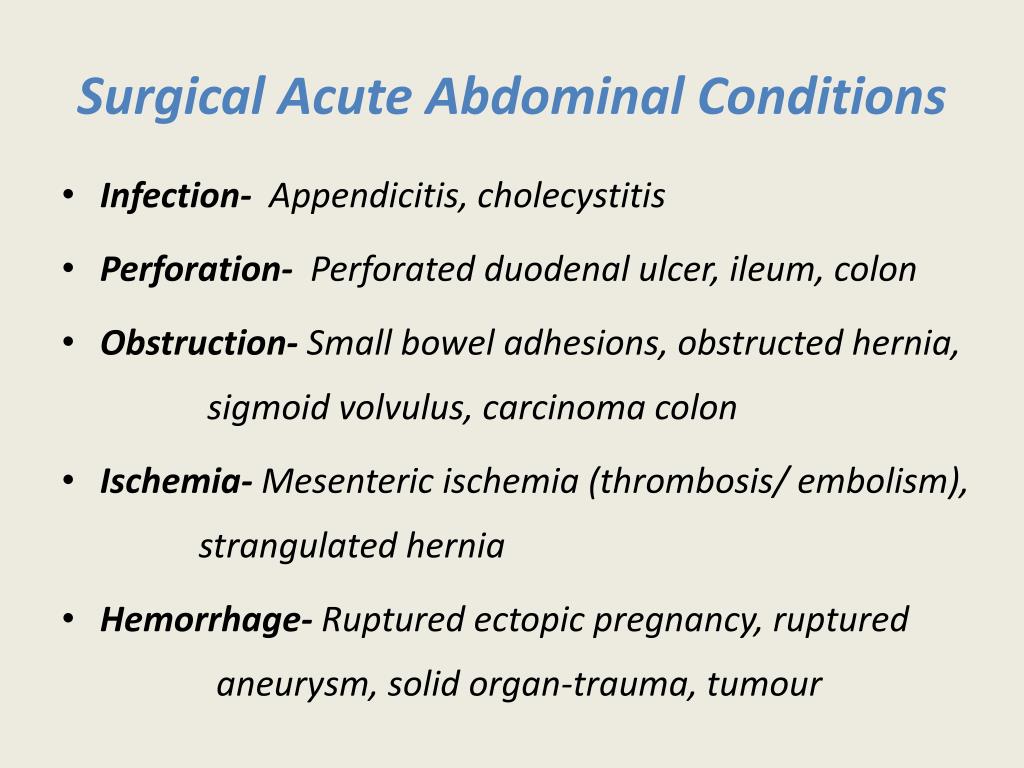
When it comes to planned abdominal surgery, several medical conditions are frequently cited as reasons for the procedure. These may include:
- Chronic digestive disorders such as Crohn's disease and ulcerative colitis
- Gallbladder diseases, particularly gallstones
- Appendicitis that necessitates appendectomy
- Hernias that require surgical repair
- Obesity and the need for bariatric surgery
- Certain cancers affecting abdominal organs
- Abdominal trauma or injury
How is the Decision Made for Planned Abdominal Surgery?
The decision to undergo planned abdominal surgery is often a collaborative process involving the patient, their family, and a team of healthcare providers. Key factors that influence this decision include:
- Severity and progression of the medical condition
- Response to non-surgical treatment options
- Potential benefits versus risks of surgery
- Patient's overall health and medical history
What Role Does a Specialist Play in the Surgical Process?
Specialists such as gastroenterologists, surgeons, and anesthesiologists play a vital role in the surgical process. They conduct thorough evaluations, recommend the best surgical options, and provide comprehensive care before, during, and after the procedure. Their expertise ensures that patients receive the highest standard of care and support throughout the surgical journey.
What Should Patients Expect Before and After Surgery?
Before surgery, patients can expect to undergo a series of pre-operative assessments that may include blood tests, imaging studies, and consultations with healthcare providers. This preparation is essential to ensure that patients are fit for surgery. After surgery, recovery protocols will vary depending on the type of procedure performed, but common elements include:
- Monitoring vital signs and managing pain
- Gradual reintroduction of food and fluids
- Physical therapy to aid in recovery
What Are the Potential Risks Associated with Planned Abdominal Surgery?
As with any surgical procedure, there are inherent risks involved with planned abdominal surgery. Potential complications may include:
- Infection at the surgical site
- Bleeding or blood clots
- Reactions to anesthesia
- Damage to surrounding organs
While the risks are present, they are often outweighed by the necessity of the procedure and its potential benefits.
How Can Patients Prepare for Planned Abdominal Surgery?
Proper preparation is key to a successful surgical outcome. Here are some tips for patients preparing for planned abdominal surgery:
- Follow pre-operative instructions provided by the healthcare team.
- Discuss any medications with the doctor, including over-the-counter supplements.
- Organize support for post-operative recovery, including transportation and assistance at home.
- Practice relaxation techniques to mitigate anxiety before the procedure.
What Are the Long-Term Outcomes of Planned Abdominal Surgery?
Long-term outcomes of planned abdominal surgery vary based on the type of surgery and the condition being treated. Many patients experience significant improvements in their quality of life, including:
- Relief from chronic pain or discomfort
- Improved digestive function
- Enhanced overall health and wellbeing
What Should You Discuss with Your Doctor Before Surgery?
Before undergoing planned abdominal surgery, it is essential to have an open dialogue with your healthcare provider. Important topics to discuss include:
- Your medical history and any allergies
- The specific details of the surgical procedure
- Potential risks and benefits
- Post-operative care and recovery expectations
Conclusion: Understanding Planned Abdominal Surgery Reasons
In summary, planned abdominal surgery can be a critical intervention for a wide range of medical conditions. Understanding the planned abdominal surgery reasons can help patients make informed decisions, prepare adequately, and navigate the recovery process more effectively. By engaging with healthcare professionals and actively participating in discussions about their health, patients can approach surgery with greater confidence and clarity.
ncG1vNJzZmirn521b6%2FOpmasp5idu6bD0qCcq7FjZL2trc2nnJ1lkZexsLnIp5ilZaOqv6ix0bJkq52RqLyvv42hq6ak